Staying strong after 40 is not optional—it’s essential. Start with what you can do, build a routine, and never ignore pain or stiffness.
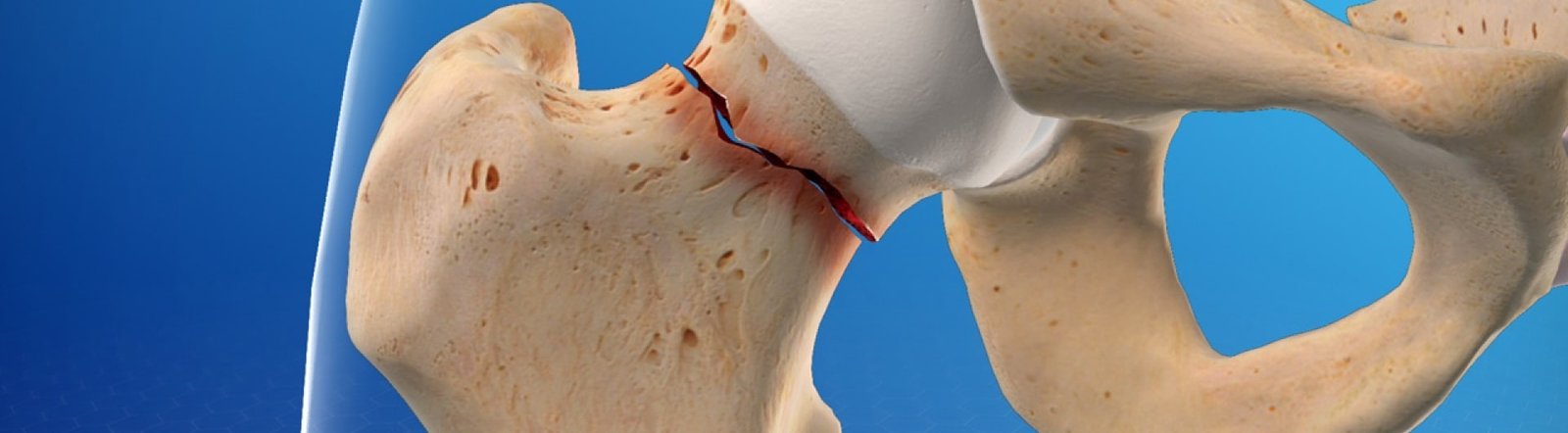
Bipolar hip replacement is a type of hip arthroplasty used primarily to treat fractures of the femoral neck or
specific degenerative conditions of the hip joint. Unlike a total hip replacement, it involves replacing only the
femoral head and leaving the acetabulum intact.
It is a type ofhemiarthroplasty , meaning only one part of the joint is replaced.
The prosthesis has two articulating surfaces:
Inner Bearing: Between the metal femoral head and a polyethylene liner.
Outer Bearing: Between the metal head and the acetabulum.
This dual articulation aims to reduce wear, provide greater mobility, and decrease the risk of acetabular erosion
compared to unipolar prostheses.
Displaced femoral neck fractures, particularly in elderly patients with low
activity levels or poor bone quality.
Avascular necrosis (AVN) of the femoral head.
Certain cases of hip arthritis, especially when acetabular involvement is minimal.
Proximal femoral lesions requiring reconstruction.
In some cases of failed previous hip surgeries.
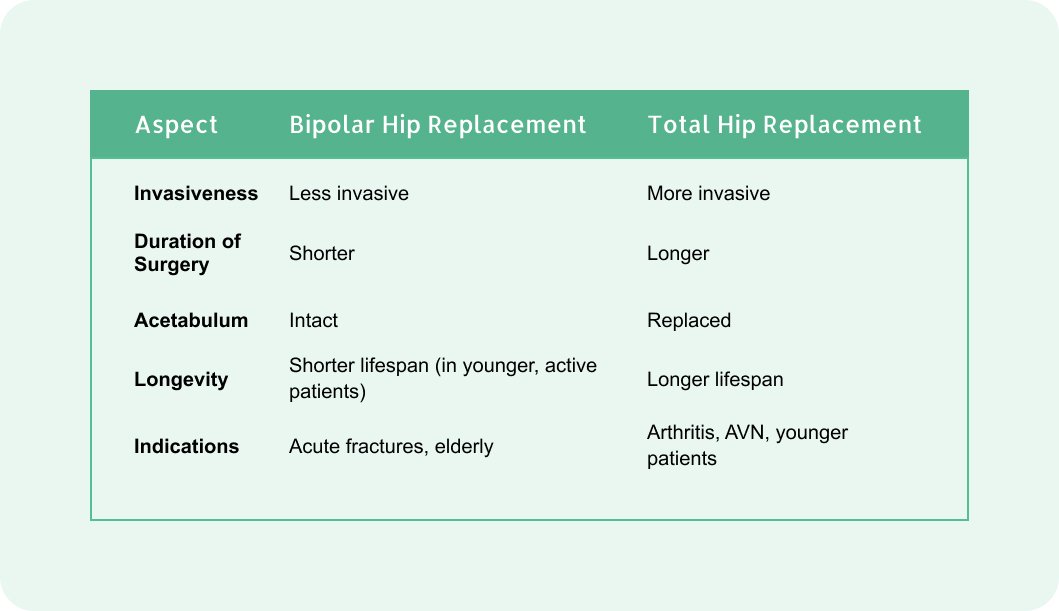
Shorter surgical time compared to total hip replacement.
Preserves the acetabulum, reducing the risk of complications associated with its prosthetic replacement.
Less invasive and better suited for elderly patients or those with multiple comorbidities.
Reduced risk of dislocation due to the dual articulation.
Anesthesia: General or regional (spinal/epidural).
Incision: A standard posterior, lateral, or anterior approach.
Femoral Head Replacement: The damaged femoral head is removed, and the prosthesis is implanted.
Articulation: The bipolar implant allows motion both within the prosthesis and between the prosthesis and
acetabulum.
Closure: The incision is sutured, and a drain may be placed.
Typically 2–4 days depending on the patient's recovery.
Early mobilization with weight-bearing as tolerated (usually within 24–48 hours).
Physical therapy for muscle strengthening and restoring range of motion.
Pain management (NSAIDs, acetaminophen).
Anticoagulants to prevent deep vein thrombosis (DVT).
Antibiotics to prevent infection.
Regular follow-up with X-rays to monitor the implant position and function.
Infection.
Hematoma formation.
Nerve or vessel injury.
Dislocation (less common due to the bipolar design).
Acetabular erosion.
Prosthesis loosening or failure.


Copyright © 20November 10, 2024 Dr. kanav's Joint Wellness Clinic . All Right Reserved